Tuesday, 31 May 2011
Thursday, 26 May 2011
Glomerular Nephritis (PBL)
Glomerulonephritis
Last reviewed: August 12, 2009.
Glomerulonephritis is a type of kidney disease in which the part of your kidneys that helps filter waste and fluids from the blood is damaged.
Causes, incidence, and risk factors
Glomerulonephritis may be caused by specific problems with the body's immune system. Often, the precise cause of glomerulonephritis is unknown.
Damage to the glomeruli causes blood and protein to be lost in the urine.
The condition may develop quickly, with loss of kidney function occurring over weeks and months (called rapidly progressive glomerulonephritis).
In about a quarter of people with chronic glomerulonephritis there is no history of kidney disease and the disorder first appears as chronic renal failure.
The following increase your risk of developing this condition:
History of cancer
Blood or lymphatic system disorders
Exposure to hydrocarbon solvents
Infections such as strep infections, viruses, heart infections,or abscesses
Diabetes
Many conditions are known to cause or increase the risk for glomerulonephritis, including:
Blood vessel diseases such as vasculitis or polyarteritis
Amyloidosis
Symptoms
Common symptoms of glomerulonephritis are:
Blood in the urine (dark, rust-colored, or brown urine)
Foamy urine
Swelling (edema) of the face, eyes, ankles, feet, legs, or abdomen
Symptoms that may also appear include the following:
Cough
Diarrhea
Fever
Joint aches
Muscle aches
Loss of appetite
Shortness of breath
Chronic renal failure symptoms may gradually develop.
Other symptoms that may occur with this disease:
Blood in the vomit or in stools
Signs and tests
Because symptoms develop gradually, the disorder may be discovered when there is an abnormal urinalysis during a routine physical or examination for unrelated disorders.
Glomerulonephritis can cause high blood pressure. It may only be discovered as a cause of high blood pressure that is difficult to control.
Laboratory tests may reveal anemia or show signs of reduced kidney functioning. A kidney biopsy confirms the diagnosis.
Later, signs of chronic kidney failure may be seen, including swelling (edema), polyneuropathy, and signs of fluid overload, including abnormal heart and lung sounds.
Imaging tests that may be done include:
Urinalysis and other urine tests include:
Examination of the urine under a microscope
This disease may also affect the results of the following blood tests:
Anti-glomerular basement membrane antibody test
Anti-neutrophil cytoplasmic antibodies (ANCAs)
BUN and creatinine
Complement levels
Treatment
Treatment varies depending on the cause of the disorder, and the type and severity of symptoms. High blood pressure may be difficult to control, and it is generally the most important aspect of treatment.
Medicines that may be prescribed include:
Blood pressure medications are often needed to control high blood pressure. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are most commonly prescribed.
Corticosteroids may relieve symptoms in some cases.
Medications that suppress the immune system may also be prescribed, depending on the cause of the condition.
A procedure called plasmapheresis may be used for some cases of glomerulonephritis due to immune-related causes. The fluid part of the blood containing antibodies is removed and replaced with intravenous fluids or donated plasma (without antibodies). Removing antibodies may reduce inflammation in the kidney tissues.
Dietary restrictions on salt, fluids, protein, and other substances may be recommended.
Persons with this condition should be closely watched for signs that they are developing kidney failure. Dialysis or a kidney transplant may eventually be necessary.
Support Groups
You can often ease the stress of illness by joining support groups where members share common experiences and problems.
Expectations (prognosis)
Glomerulonephritis may be a temporary and reversible condition, or it may get worse. Progressive glomerulonephritis may lead to chronic kidney failure and end-stage kidney disease.
If you have nephrotic syndrome and it can be controlled, other symptoms may also be controlled. If it can't be controlled, end-stage kidney disease may result.
Complications
Chronic kidney failure
End-stage kidney disease
Fluid overload -- congestive heart failure, pulmonary edema
Increased susceptibility to other infections
Calling your health care provider
Call your health care provider if:
You have disorders that are associated with an increased risk of glomerulonephritis
You develop symptoms of glomerulonephritis
Prevention
There is no specific way to prevent most cases of glomerulonephritis. Some cases may be prevented by avoiding or limiting exposure to organic solvents, mercury, and nonsteroidal anti-inflammatory drugs (NSAIDs).
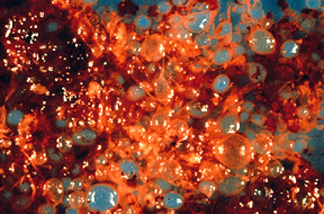
POLYCYSTIC KIDNEY
Polycystic kidney disease (PKD) is a disorder in which clusters of cysts develop primarily within your kidneys. Cysts are noncancerous round sacs containing water-like fluid.
Polycystic kidney disease isn't limited to only kidneys, although the kidneys usually are the most severely affected organs. The disease can cause cysts to develop elsewhere in body.
The greatest risk for people with polycystic kidney disease is developing high blood pressure. Kidney failure is another common problem for people with polycystic kidney disease.
Polycystic kidney disease varies greatly in its severity, and some complications are preventable. Regular checkups can lead to treatments to reduce damage to kidneys from complications, such as high blood pressure.
Cysts are noncancerous (benign), round sacs that contain water-like fluid. They vary in size and as they accumulate more fluid can grow extremely large. A kidney containing numerous cysts can weigh as much as 30 pounds.
Abnormal genes cause polycystic kidney disease, and the genetic defects mean the disease runs in families. There are two types of polycystic kidney disease, caused by different genetic flaws:
- Autosomal dominant polycystic kidney disease (ADPKD). Signs and symptoms of ADPKD often develop between the ages of 30 and 40. In the past, this type was called adult polycystic kidney disease, but children can develop the disorder. Only one parent needs to have the disease in order for it to pass along to the children. If one parent has ADPKD, each child has a 50 percent chance of getting the disease. This form accounts for about 90 percent of cases of polycystic kidney disease.
- Autosomal recessive polycystic kidney disease (ARPKD). This type is far less common than ADPKD. The signs and symptoms often appear shortly after birth. Sometimes, symptoms don't appear until later in childhood or during adolescence. Both parents must have abnormal genes to pass on this form of the disease. If both parents carry the genes for this disorder, each child has a 25 percent chance of getting the disease.
Researchers have identified two genes associated with ADPKD and one associated with ARPKD so far.
In some cases, a person with ADPKD has no known family history of the disease. But it's possible that someone in the affected person's family actually did have the disease, but didn't show signs or symptoms before dying of other causes. In a smaller percentage of cases where no family history is present, ADPKD results from a spontaneous gene mutation.
SYMPTOMPS
Polycystic kidney disease symptoms may include:
- High blood pressure
- Back or side pain related to enlarged kidneys
- Headache
- Increase in the size of your abdomen
- Blood in your urine
- Frequent urination
- Kidney stones
- Kidney failure
- Urinary tract or kidney infections
- High blood pressure. Elevated blood pressure is a common complication of polycystic kidney disease. Untreated, high blood pressure can cause further damage to your kidneys and increase your risk of heart disease and stroke.
-
Loss of kidney function. Progressive loss of kidney function is one of the most serious complications of polycystic kidney disease. Nearly half of those with the disease have kidney failure by age 60, and up to 75 percent have kidney failure by age 70. If you have high blood pressure or blood or protein in your urine, you have a greater risk of kidney failure.
Polycystic kidney disease causes your kidneys to gradually lose their ability to eliminate wastes from your blood and maintain your body's balance of fluids and chemicals. As the cysts enlarge, they produce pressure and promote scarring in the normal, unaffected areas of your kidneys. These effects result in high blood pressure and interfere with the ability of your kidneys to keep wastes from building to toxic levels, a condition called uremia. As the disease worsens, end-stage kidney (renal) failure may result. When end-stage renal failure occurs, you'll need ongoing kidney dialysis or a transplant to prolong your life.
- Pregnancy complications. Pregnancy is successful for most women with polycystic kidney disease. In some cases, however, women may develop a life-threatening disorder called preeclampsia. Those most at risk are women who have high blood pressure before they become pregnant.
- Growth of cysts in your liver. The likelihood of developing liver cysts for someone with polycystic kidney disease increases with age. While both men and women develop cysts, women often develop larger cysts. Cyst growth may be aided by female hormones.
- Development of an aneurysm in your brain. Localized enlargement of an artery in your brain can cause a hemorrhage if it ruptures. People with polycystic kidney disease have a higher risk of aneurysm, especially those that occur before age 50. The risk is higher if you have a family history of aneurysm or if you have uncontrolled high blood pressure.
- Heart valve abnormalities. As many as one-quarter of adults with polycystic kidney disease develop mitral valve prolapse. When this happens, the valve no longer closes properly, which allows blood to leak backward.
- Colon problems. Hernias and pouches or sacs in the wall of the colon (diverticulosis) may develop in people with polycystic kidney disease.
- Chronic pain. Pain is a common symptom for people with polycystic kidney disease. It often occurs in your side or back. The pain also can be associated with a urinary tract infection or a kidney stone.
Saturday, 7 May 2011
Female Reproductive Quizzes

a. acute salpingitis
b. adenocarcinoma
c. ectopic preganancy
d. it's normal
The correct answer is ectopic Pregnancy
Question 2
This large encapsulated myometrial tumor is most consistent with
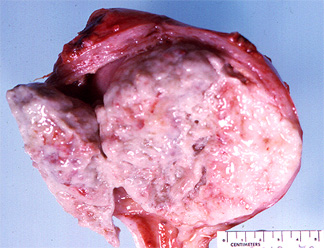
a. a leiomyoma
b. endometrial carcinoma
c. a former placental implantation site
d. a teratoma
A Liomyoma
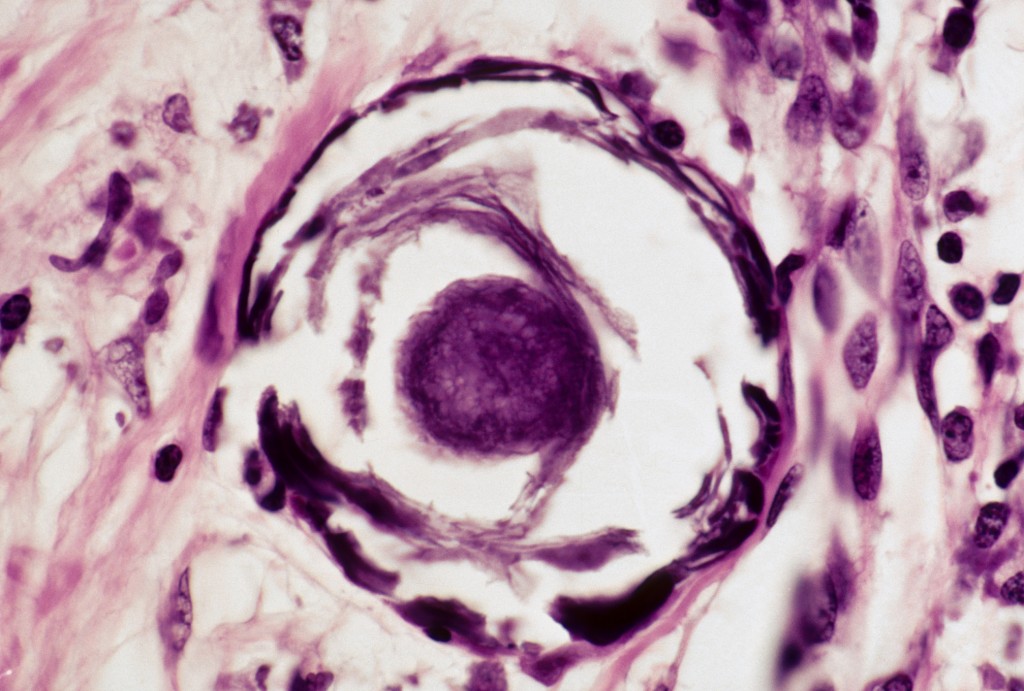
Question 3
The following two photographs are of a vulvar lesion from a 61 year old woman. They are most most consistent with
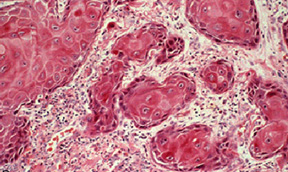

a. a staphylococcal infection
b. a leiomyoma of the skin
c. endometriosis
d. invasive squamous cell carcinoma
The correct answer is: d
Question 4
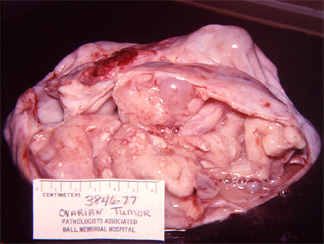
This cystic ovarian tumor
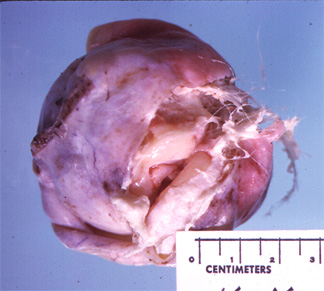
a. is almost certainly malignant
b. could be the source of ectopic thyroid hormone
c. is likely producing Beta HCG
d. is an example of endometriosis
The correct answer is: b
Question 5
A 32 year-old female had a cervical punch biopsy following an abnormal Pap smear. Based on the histology, which of the following should be done?

a. cervical cone biopsy
b. antibiotic therapy with repeat punch biopsy in three months
c. hysterectomy with lymph node dissection
d. topical estrogen therapy
The correct answer is: a
Question 6
The following picture is of a large, multicloculated mucinous cystadenoma of the ovary. Tumors of this type are known what tumor marker or hormome?
a. Beta HCG
b. progesterone
c. Alpha fetoprotein
d. These tumors produce no homrome or marker.
The correct answer is: d
Question 7
The following phototographs are of a tissue from a D&C of a woman who was thought to be pregnant but had spontaneously aborted. The circled area highlights atypical trophoblastic material. The surgical report described the tissue as looking like a cluster of grapes. Follow up of this woman must include
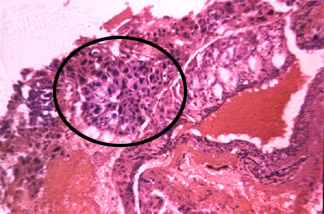
a. Serial Beta HCG determinations.
b. Since she has aborted, no follow up is needed.
c. A one time serum estrogen level.
d. Serial PAP smears at least monthly for the next six months.
The correct answer is: a
Question 8
The woman from the previous question continued to experience vaginal bleeding and was shown to have markedly elevated Beta HCG levels several weeks following the spontaneous abortion. Surgery was needed and the following picture is of her uterus. Given the history, the highlighted area is most consistent with
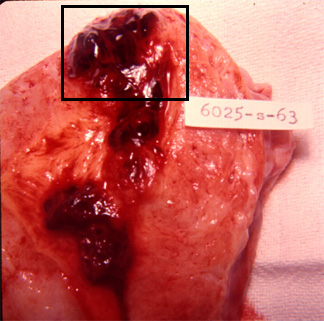
a. a leiomyoma
b. an invasive mole
c. adenocarcinoma of the endometrium
d. metastatic cervical cell carcinoma
The correct answer is: b
Question 9
Carcinoma of the cervix usually begins at the junction of the.
a. ectocervix and endocervix
b. endocervix and endometrium
c. deep and superficial endocervical glands
d. vagina and cervix
The correct answer is: a
Question 10
Except for one pregnancy during her mid twenties, this 51 year-old woman had had regular menstrual periods since the age of 15 until one year ago. At that time she began to have intermenstrual bleeding. This has increased in frquency and severity so that during most of the last month there has been some spotting each day and several times bleeding was profuse. Physical examination revealed left adnexal mass the size of a grapefruit and a small trickle of blood coming from the cervical os. A diagnostic D & C was performed.
The disease process which best characterizes this picture is
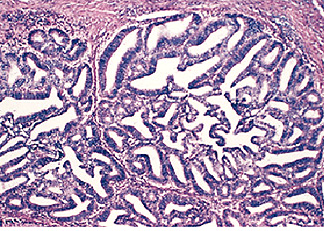
a. secretory endometrium
b. hyperplasia of endometrium
c. adenocarcinoma of endometrium
d. products of conception
The correct answer is: c
Wednesday, 4 May 2011
What were once sins are now a disease
*PATHOLOGY: Sometimes what is defined as unusual is seen as a medical problem
(i.e. an illness) other times it is defined as falling within the realm of
religion or law (i.e. as sin or deviant).
A Brief History of Western Medical Practice:
* In the beginning, illness was defined in religious terms as a spiritual
problem (e.g. Egypt, Mesopotamia, early Greece)
* Hippocrates moved to secularize disease & base medicine on empirical
observation. Introduced idea of balance.
* Galen: functional view of organs: influential anatomical works
* Medieval period: medical science declined: religious thought again
dominant
* Great plagues: ideas raised about quarantine, germ theory & case
histories
* 18th century: re-emergence of scientific medicine: age of medical
discoveries/ organization of medical knowledge vs. competing cures
* Secularization of the body, separation of church & state, + growth in
individual rights enabled clearer distinctions between disease, deviance,
crime, & sin
* Various experiments/discoveries/ advances in surgery, accompanied by various practices seen as harmful today.
Effects of Medicalization on mankind
* Upside: labelling something an illness more humanitarian than
blaming
* Downsides:
- Removing responsibility from individuals in favor of "disorder"
-Veiling political nature of negative judgement under guise of
scientific fact
- The problem of "expert control"
- The individualization of social problems
- The depoliticization of victims= behavior
- The potential for medical social control
- The implicit "exclusion of evil"
Monday, 2 May 2011
Sedekah yang disebut dalam al-quran
Sunday, 1 May 2011
Tyme 4 QuIZzes
1. Which of the following is true of papillary thyroid carcinoma?
A. May have psammoma bodies
B. The least common kind of thyroid carcinoma
C. The type of thyroid carcinoma with the worst prognosis
D. Occurs in patients with MEN II
E. Most common in elderly patients
2. The most common cause of hypothyroidism in underprivileged countries is:
A. Pituitary dysfunction
B. DeQuervain’s thyroiditis
C. Graves’ disease
D. Hashimoto’s thyroiditis
E. Iodine deficiency
The answer is E, iodine deficiency. To give you an idea of the devastating effects of the disease, here is a short story about how hypothyroidism affected one child’s life. Congenital hypothyroidism is the biggest cause of preventable mental retardation in the world, and it is most prevalent in disadvantaged areas of the world. In most cases, it is simply due to a lack of iodine in the diet. Unicef is working to eliminate iodine deficiency in all parts of the world. Iodine is cheap; even a small donation will make a big difference in many children’s lives.
3. Which of the following hormones, in addition to participating in the initiation of labor, may play a role in trust, monogamy, and the desire to cuddle?
A. Cortisol
B. Thyroid hormone
C. Parathormone
D. Oxytocin
E. Antidiuretic hormone
The answer is D, oxytocin
4. A patient with Cushing syndrome might present with any of the following EXCEPT:
A. Obesity
B. A buffalo hump
C. Moon facies
D. Bronze or hyperpigmented skin
E. Glucose intolerance
All the answers except D are commonly seen in Cushing syndrome. Bronze or hyperpigmented skin is a finding seen in Addison Disease. It occurs because the pituitary is cranking out ACTH like crazy in an effort to get the adrenals to make their hormones. ACTH comes from a bigger precursor called pro-opiomelanocortin (POMC) which also gives rise to melanocyte-stimulating hormone (MSH). If you’re making more ACTH, you’re also by necessity making more MSH – and your skin will turn bronze.
5. Patients with diabetes have an increased risk of all of the following EXCEPT:
A. Cataracts
B. Infections
C. Increased atherosclerosis
D. Peripheral neuropathy
E. Pancreatic carcinoma
The big things with diabetes are infections, vascular problems, eye problems, and nerve problems. Pancreatic carcinoma doesn’t show any significant increased incidence in patients with diabetes.
7. Which of the following is true regarding pheochromocytoma?
A. It can cause hypertension
B. It is usually an aggressive, malignant tumor
C. It only occurs in the adrenal gland
D. It is derived from neural crest cells
E. Many tumors have a 1p deletion
A is correct; pheochromocytomas can definitely present with hypertension. All that catecholamine release makes your blood pressure go up. Only about 10% of cases are malignant, so B is wrong. 10% of cases are extra-adrenal, so C is wrong. It is derived from the catecholamine-producing cells of the medulla (which are neural-crest derived)- so D is correct too! Chromosome 1 is not messed up in pheochromocytoma, so E is wrong. Some patients with neuroblastoma do have a deletion of the short arm of chromosome 1. By the way, the short arm was named “p” for “petit.” Cool, huh? Also, I always remember that q stands for the long arm because the letter q has a longer tail than the letter p.
8. Which of the following is true regarding Addison’s disease?
A. It is characterized by an overproduction of catecholamines
B. Most cases are due to infection
C. It is also called primary chronic adrenal insufficiency
D. The onset is sudden
E. Patients are often hypertensive
Addison’s disease is also called primary chronic adrenal insufficiency (so C is correct). It’s primary because the problem is localized to the adrenal itself (usually it’s an autoimmune thing, not an infectioius thing, so B is wrong), and it’s chronic (slowly progressive) as opposed to acute (like Waterhouse-Friderichson Syndrome).
It is not characterized by an overproduction of catecholamines (so A is wrong), but by an underproduction of everything the adrenal cortex makes: mineralocorticoids, glucocorticoids, and sex steroids. You don’t notice the sex steroid underproduction much, but you get symptoms from the lack of mineralocorticoids and cortisol for sure.
The onset is not sudden (so D is wrong). The onset of disease is slow and progressive – it takes a long, long time for the disease to eradicate enough of the adrenal to produce symptoms. The disease might present in what seems like an acute fashion – but if you look back, you’d be able to see signs that were present for a long time (like a tanned appearance, or fatigue).
Patients are not hypertensive; if anything, they are hypotensive because the lack of mineralocorticoids leads to a drop in blood sodium, which leads to a lower blood volume and hypertension. So E is wrong.
9. You are seeing a 41-year old male who is very tall and has a large jaw. You wonder if he might have acromegaly due to a pituitary adenoma. What laboratory test would be best for making this diagnosis?
A. Insulin-like growth factor level
B. Random serum growth hormone level
C. Prolactin level
D. Hemoglobin
E. Lactate dehydrogenase
Acromegaly is caused by a growth hormone-producing pituitary adenoma. You’d think you could just measure growth hormone, but since GH happens to be secreted in a pulsatile fashion, you can’t just take a random GH measurement; you wouldn’t know where on the curve the patient was (so B is wrong). Insulin-like growth factor is a surrogate marker that is made by the liver and released in a constant, non-pulsatile fashion. It’s what is usually measured in the workup of a GH producing pituitary adenoma. So A is correct.
10. Your sister is complaining that she is always tired, despite getting enough sleep. You notice that she seems pale, and when you feel her pulse it is quite slow. She also mentions that she can’t stand the cold these days. What two lab tests would be most helpful in diagnosing her condition?
A. FSH and LH levels
B. Free T4 and TSH levels
C. Calcium, phosphate, and parathyroid hormone levels
D. Insulin-like growth factor and prolactin levels
E. Cortisol and ACTH levels
Tired all the time and pale could mean anemia. But since your sister has a slow pulse (not a fast one, like you’d expect in severe anemia) – and since that’s not one of the answers – we can rule that out.
Tired, pale, bradycardic (slow pulse) and cold is a great history for hypothyroidism. She also might feel depressed and may have gained weight recently. For hypothyroidism (or hyperthyroidism, for that matter), the best tests to get are a T4 (best to measure the free T4, because that’s the active fraction) and a TSH. The T4 is low in hypothyroidism, and if it’s a disease localized to the thyroid gland, like Hashimoto thyroiditis, the TSH will be high (because it’s responding to the puny amount of T4 put out by the thyroid gland). If the hypothyroidism is due to hypopituitarism (which is rare), then the TSH will be low (because that’s what’s driving the T4 down).
Original post: http://www.pathologystudent.com/?p=2451